
Revolutionizing Healthcare: Patient Engagement Software And Practice Management
The Journey of Integrating Electronic Health Records (EHR)
The journey of integrating electronic health records (EHR) within healthcare systems has been transformative, offering a unified platform for record-keeping. With real-time updates and centralization, EHRs reduce redundancy, ensuring seamless communication between healthcare professionals. Surprising though it may be, EHR implementation has compressed patient data accessibility, improving decision-making and treatment outcomes.
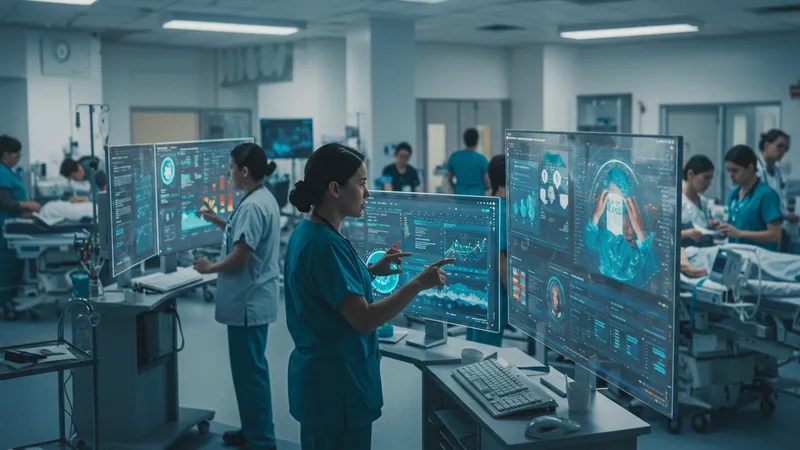
EHRs streamline operations and alleviate administrative burdens on healthcare staff, enabling them to focus more on patient care. The efficiency of electronic records is indisputable, cutting down documentation times drastically. Interestingly, hospitals using EHR systems report a reduction in medical errors, reinforcing safety protocols across clinical practices.
The integration process, however, is not without challenges. Institutions frequently encounter resistance from staff used to traditional record-keeping methods. Retraining medical personnel to fully utilize digital tools is vital to unlocking EHRs’ full potential. Overcoming this hurdle is critical to the successful realization of electronic health records’ aims, from accuracy to accessibility improvements.
Despite obstacles, the EHR movement is moving rapidly toward an interconnected healthcare ecosystem. The question arises: how can institutions ensure continued innovations in the EHR space while maintaining patient confidentiality and data security? The answer to this question lies at the heart of ongoing industry reform, drawing the roadmap for EHR practices worldwide.





